TBI and Concussion: Signs, Symptoms & Help
UNDERSTANDING TBI AND CONCUSSION:
Signs and Symptoms and Help: The Basics of Recovery
A concussion or traumatic brain injury (TBI) is caused by a bump, blow, or jolt to the head that can change the way your brain normally works. Concussions can also occur from a fall or a blow to the body that causes the head and brain to move quickly back and forth. Concussions may be described as a “mild” brain injury because they are usually not life-threatening. Even so, their effects can be serious.
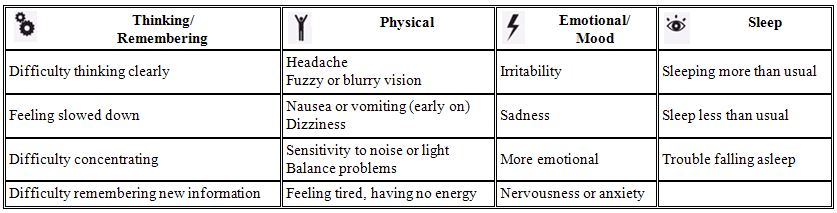
Signs and Symptoms of a concussion usually fall into four categories:
When to Seek Immediate Medical Attention
What Should I do If a Concussion Occurs?
What Should I do If a Concussion Occurs while Playing Sports?
General Tips to Help Aid in Recovery
Return to Play/School Progression – Children, Students, Adults, Athletes
Help Prevent Long-Term Problems
What are the Potential Long-Term Outcomes of TBI
What Can I do to Help Prevent Concussion and other forms of TBI?
Severe Traumatic Brain Injury
Potential Effects of Severe TBI
Fast Facts
When to Seek Immediate Medical Attention:
Danger Signs in Adults
In rare cases, a dangerous blood clot may form on the brain in a person with a concussion and crowd the brain against the skull. Contact your health care professional or emergency department right away if you have any of the following danger signs after a bump, blow, or jolt to the head or body:
- Headache that gets worse and does not go away.
- Weakness, numbness or decreased coordination.
- Repeated vomiting or nausea.
- Slurred speech.
The people checking on you should take you to an emergency department right away if you:
- Look very drowsy or cannot be awakened.
- Have one pupil (the black part in the middle of the eye) larger than the other.
- Have convulsions or seizures.
- Cannot recognize people or places.
- Are getting more and more confused, restless, or agitated.
- Have unusual behavior.
- Lose consciousness (a brief loss of consciousness should be taken seriously and the person should be carefully monitored).
Danger Signs in Children
Take your child to the emergency department right away if they received a bump, blow, or jolt to the head or body, and:
- Have any of the danger signs for adults listed above.
- Will not stop crying and cannot be consoled.
- Will not nurse or eat.
Some of these symptoms may appear right away, while others may not be noticed for days or months after the injury, or until the person starts resuming their everyday life and more demands are placed upon them. Sometimes, people do not recognize or admit that they are having problems. Still, others may not understand why they are having problems and what their problems really are, which can make them nervous and upset.
Most people with a TBI recover quickly and fully. But for some people, symptoms can last for days, weeks, or longer. In general, recovery may be slower among older adults, young children, and teens. Those who have had a TBI in the past are also at risk of having another one and may find that it takes longer to recover if they have another TBI.
Back to Top
What Should I do If a Concussion Occurs?
If you think you or someone you know has a TBI, contact your health care professional. Getting help soon after the injury by trained specialists may speed recovery.
In addition to seeking medical attention, the Brain Health Education and Research Institute recommends adding the Dr. Lewis Omega-3 Protocol to your treatment regimen.
What Should I do If a Concussion Occurs While Playing Sports?
If you suspect that an athlete has a concussion, implement the 4-step action plan:
- Remove the athlete from play. Look for signs and symptoms of a concussion if the athlete has experienced a bump or blow to the head or body. When in doubt, keep the athlete out of play.
- Ensure that the athlete is evaluated by a health care professional experienced in evaluating for concussion. Do not try to judge the severity of the injury yourself. Health care professionals have a number of methods that they can use to assess the severity of concussions. As a coach or parent, recording the following information can help health care professionals in assessing the athlete after the injury:
- Cause of the injury and force of the hit or blow to the head or body
- Any loss of consciousness (passed out/knocked out) and if so, for how long
- Any memory loss immediately following the injury
- Any seizures immediately following the injury
- Number of previous concussions (if any)
- Inform the athlete’s parents or guardians about the possible concussion and give them the CDC’s fact sheet on concussion. Make sure they know that the athlete should be seen by a health care professional experienced in evaluating for concussion.
- Keep the athlete out of play the day of the injury and until a health care professional, experienced in evaluating for concussion, says they are symptom-free and it’s OK to return to play. A repeat concussion that occurs before the brain recovers from the first—usually within a short period of time (hours, days, or weeks)—can slow recovery or increase the likelihood of having long-term problems. In rare cases, repeat concussions can result in edema (brain swelling), permanent brain damage, and even death.
General Tips to Help Aid in Recovery:
- Get lots of rest. Don’t rush back to daily activities such as work, school, or sports.
- For children, make sure they get plenty of rest. Keep a regular sleep schedule, including no late nights and no sleepovers.
- Avoid doing anything that could cause another blow or jolt to the head, especially contact or recreational sports that could lead to another concussion.
- Making sure children avoid high-risk/ high-speed activities such as riding a bicycle, playing sports, or climbing playground equipment, roller coasters or rides that could result in another bump, blow, or jolt to the head or body.
- Ask your health care professional when it’s safe to drive a car, ride a bike, or use heavy equipment, because your ability to react may be slower after a brain injury.
- Avoid activities that are physically demanding (e.g., heavy housecleaning, weightlifting/working-out) or require a lot of concentration (e.g., balancing your checkbook). They can make your symptoms worse and slow your recovery.
- Take only the drugs your health care professional has approved, and don’t drink alcohol until your health care professional says it’s OK.
- Write things down if you have a hard time remembering and consult with family members or close friends when making important decisions.
- You may need help to re-learn skills that were lost. Your health care professional can help arrange for these services.
- Avoid sustained computer use, including computer/video games early in the recovery process.
- Some people report that flying in airplanes makes their symptoms worse shortly after a concussion.
- When your health care professional says you are well enough, return to your normal activities gradually, not all at once.
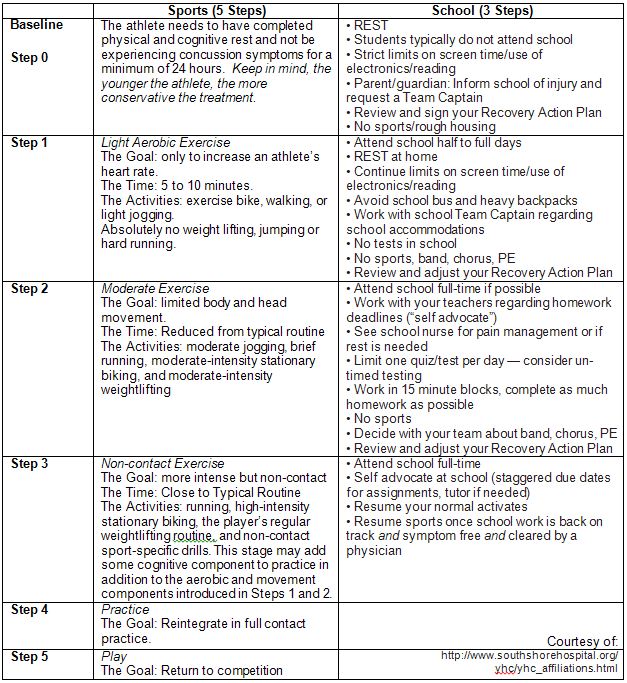
Return to Play/School Progression – this applies not just to athletes, but to children, students, and adults.
For specific information about Return-to-School guidelines, please go to http://www.cdc.gov/concussion/pdf/TBI_Returning_to_School-a.pdf or http://www.southshorehospital.org/yhc/yhc_affiliations.html
It is important to monitor symptoms and cognitive function carefully during each increase of exertion. Athletes and students should only progress to the next level if they are not experiencing symptoms at the current level. If symptoms return at any step, they should stop these activities as this may be a sign they are pushing too hard. Only after additional rest, when the person is once again not experiencing symptoms for a minimum of 24 hours, should he or she start again at the previous step during which symptoms were experienced.
The Return to Play Progression process is best conducted through a team approach and by a health professional who knows the student or athlete’s abilities and endurance. By gauging the their performance on each individual step, a health care professional will be able to determine how far to progress the patient on a given day. In some cases, the person may be able to work through one step in a single day, while in other cases it may take several days to work through an individual step. It may take days to months to work through the entire 5-step progression.
Remember, while most people will recover quickly and fully following a concussion, some will have symptoms for weeks or longer. Health care professionals should consider referral to a concussion specialist if:
- the symptoms worsen at any time,
- symptoms have not gone away after 10-14 days, or
- the patient has a history of multiple concussions or risk factors for prolonged recovery. This may include a history of migranes, depression, mood disorders, or anxiety, as well as developmental disorders such as learning disabilities and ADHD.
Help Prevent Long-Term Problems
On rare occasions, receiving another concussion before the brain has healed can result in brain swelling, permanent brain damage, and even death, particularly among children and teens. If you already had a medical condition at the time of your concussion (such as chronic headaches), it may take longer for you to recover from the concussion. Anxiety and depression may also make it harder to adjust to the symptoms of a concussion.
After you have recovered from your concussion, you should protect yourself from having another one. People who have had repeated concussions may have serious long-term problems, including chronic difficulty with concentration, memory, headache, and occasionally, physical skills, such as keeping one’s balance.
What are the Potential Long-Term Outcomes of TBI?
The severity of a TBI may range from mild (a brief change in mental status or consciousness) to severe (an extended period of unconsciousness or amnesia after the injury). TBI can cause a wide range of functional short- or long-term changes in:
- Thinking (i.e., memory and reasoning);
- Sensation (i.e., touch, taste, and smell);
- Language (i.e., communication, expression, and understanding); and
- Emotion (i.e., depression, anxiety, personality changes, aggression, acting out, and social inappropriateness).1
TBI can also cause epilepsy and increase the risk for conditions such as Alzheimer’s disease, Parkinson’s disease, and other brain disorders that become more prevalent with age.1
Repeated mild TBIs occurring over an extended period of time (i.e., months, years) can result in cumulative neurological and cognitive deficits. Repeated mild TBIs occurring within a short period of time (i.e., hours, days, or weeks) can be catastrophic or fatal.3
- National Institute of Neurological Disorders and Stroke. Traumatic brain injury: hope through research. Bethesda (MD): National Institutes of Health; 2002 Feb. NIH Publication No.: 02-158.
- Centers for Disease Control and Prevention (CDC), National Center for Injury Prevention and Control. Report to Congress on mild traumatic brain injury in the United States: steps to prevent a serious public health problem. Atlanta (GA): Centers for Disease Control and Prevention; 2003.
- Centers for Disease Control and Prevention (CDC). Sports-related recurrent brain injuries—United States. MMWR 1997;46(10):224–227.
- Centers for Disease Control and Prevention (CDC). Facts about concussion and brain injury: Where to Get Help. 2010.
What Can I do to Help Prevent Concussion and other forms of TBI?
There are many ways to reduce the chances of a concussion or TBI, including:
- Wearing a seat belt every time you drive or ride in a motor vehicle.
- Buckling your child in the car using a child safety seat, booster seat, or seat belt (according to the child’s height, weight, and age).
- Children should start using a booster seat when they outgrow their child safety seats (usually when they weigh about 40 pounds). They should continue to ride in a booster seat until the lap/shoulder belts in the car fit properly, typically when they are 4’9” tall.1
- Never driving while under the influence of alcohol or drugs.
- Wearing a helmet and making sure your children wear helmets when:
- Riding a bike, motorcycle, snowmobile, scooter, or all-terrain vehicle;
- Playing a contact sport, such as football, ice hockey, or boxing;
- Using in-line skates or riding a skateboard;
- Batting and running bases in baseball or softball;
- Riding a horse; or
- Skiing or snowboarding.
- Making living areas safer for seniors, by:
- Removing tripping hazards such as throw rugs and clutter in walkways;
- Using nonslip mats in the bathtub and on shower floors; Installing grab bars next to the toilet and in the tub or shower;
- Installing handrails on both sides of stairways;
- Improving lighting throughout the home; and
- Maintaining a regular physical activity program, if your doctor agrees, to improve lower body strength and balance.2,3,4
- Making living areas safer for children, by:
- Installing window guards to keep young children from falling out of open windows; and
- Using safety gates at the top and bottom of stairs when young children are around.
- Making sure the surface on your child’s playground is made of shock-absorbing material, such as hardwood mulch or sand.5
References
- Centers for Disease Control and Prevention. Warning on interaction between air bags and rear-facing child restraints. Morbidity and Mortality Weekly Report MMWR 1993;42(No.14):20–22.
- Judge JO, Lindsey C, Underwood M, Winsemius D. Balance improvements in older women: effects of exercise training. Physical Therapy 1993;73(4):254–265.
- Lord SR, Caplan GA, Ward JA. Balance, reaction time, and muscle strength in exercising older women: a pilot study. Archives of Physical and Medical Rehabilitation 1993;74(8):837–839.
- Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age and Aging 1999;28:513–518.
- Mack MG, Sacks JJ, Thompson D. Testing the impact attenuation of loose fill playground surfaces. Injury Prevention 2000;6:141–144.
Severe Traumatic Brain Injury
Each year, TBIs contribute to a substantial number of deaths and cases of permanent disability. A severe TBI not only impacts the life of an individual and their family, but it also has a large societal and economic toll. The estimated economic cost of TBI in 2010, including direct and indirect medical costs, is estimated to be approximately $76.5 billion. Additionally, the cost of fatal TBIs and TBIs requiring hospitalization, many of which are severe, account for approximately 90% of the total TBI medical costs. (2,3)
The Glasgow Coma Scale (GCS)(4), a clinical tool designed to assess coma and impaired consciousness, is one of the most commonly used severity scoring systems. Persons with GCS scores of 3 to 8 are classified with a severe TBI, those with scores of 9 to 12 are classified with a moderate TBI, and those with scores of 13 to 15 are classified with a mild TBI. Other classification systems include the Abbreviated Injury Scale (AIS), the Trauma Score, and the Abbreviated Trauma Score. Despite their limitations(5), these systems are crucial to understanding the clinical management and the likely outcomes of this injury as the prognosis for milder forms of TBIs is better than for moderate or severe TBIs.(6-8)
Potential effects of Severe TBI
A non-fatal severe TBI may result in an extended period of unconsciousness (coma) or amnesia after the injury. For individuals hospitalized after a TBI, almost half (43%) have a related disability one year after the injury.(9) A TBI may lead to a wide range of short- or long-term issues affecting:
- Cognitive Function (e.g., attention and memory)
- Motor function (e.g., extremity weakness, impaired coordination and balance)
- Sensation (e.g., hearing, vision, impaired perception and touch)
- Emotion (e.g., depression, anxiety, aggression, impulse control, personality changes)
Approximately 5.3 million Americans are living with a TBI-related disability and the consequences of severe TBI can affect all aspects of an individual’s life.(10) This can include relationships with family and friends, as well as their ability to work or be employed, do household tasks, drive, and/or participate in other activities of daily living.
As with most diseases and injuries, the best approach to severe TBI is prevention. Once a severe TBI occurs, the road to recovery can be long and difficult, not only for the patient, but also for their families and caregivers. While great strides have been made in the past decade in the area of acute care and surgical care of severe TBI, the reality is that the long term care hasn’t really changed in centuries.
Back to Top
Fast Facts
Falls are the leading cause of TBI and recent data shows that the number of fall-related TBIs among children aged 0-4 years and in older adults aged 75 years or older is increasing.
Among all age groups, motor vehicle crashes and traffic-related incidents result in the largest percentage of TBI-related deaths (31.8%).(1)
People aged 75 years old and older have the highest rates of TBI-related hospitalizations and death.(1)
Shaken Baby Syndrome (SBS), a form of abusive head trauma (AHT) and inflicted TBI, is a leading cause of child maltreatment deaths in the United States.
References
- Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010.
- Finkelstein E, Corso P, Miller T and associates. The Incidence and Economic Burden of Injuries in the United States. New York (NY): Oxford University Press; 2006.
- Coronado, McGuire, Faul, Sugerman, Pearson. The Epidemiology and Prevention of TBI (in press) 2012
- Teasdale, G, Jennett, B. Assessment of coma and impaired consciousness. A practical scale. Lancet 304(7872):81-84, 1974.
- Stein SC. Classification of head injury. In: Narayan, RK, Wilberger, Jr., JE, Povlishock, JT, eds. Neurotrauma. McGraw-Hill, 1996:31-41.
- Coronado, VG, Thurman, DJ, Greenspan, AI, et al. Epidemiology. In: Jallo, J, Loftus, C, eds. Neurotrauma and Critical Care of the Brain. New York, Stuttgart: Thieme, 2009.
- Levin, HS, Gary, HE, Eisenberg, HM, et al. Neurobehavioral outcome 1 year after severe head injury. Experience of the Traumatic Coma Data Bank. J Neurosurg 73(5):699-709, 1990.
- Williams, DH, Levin, HS, Eisenberg, HM. Mild head injury classification. Neurosurgery 27(3):422-428, 1990.
- Selassie AW, Zaloshnja E, Langlois JA, Miler T, Jones P, Steiner C. Incidence of Long-term disability following Traumatic Brain Injury Hospitalization, United States, 2003 J Head Trauma Rehabil 23(2):123-131,2008.
- Thurman D, Alverson C, Dunn K, Guerrero J, Sniezek J. Traumatic brain injury in the United States: a public health perspective. J Head Trauma Rehabil 1999;14(6):602-615.
MINOR MODIFICATIONS FROM ORIGINAL SOURCE: WWW.CDC.GOV/CONCUSSION
Back to Top